Pippa was diagnosed with vulvar cancer in January 2023, but her story began months earlier with subtle symptoms that wouldn’t resolve. Persistent soreness and discomfort lingered despite over-the-counter treatments. While nothing seemed urgent at first, Pippa felt something wasn’t right.
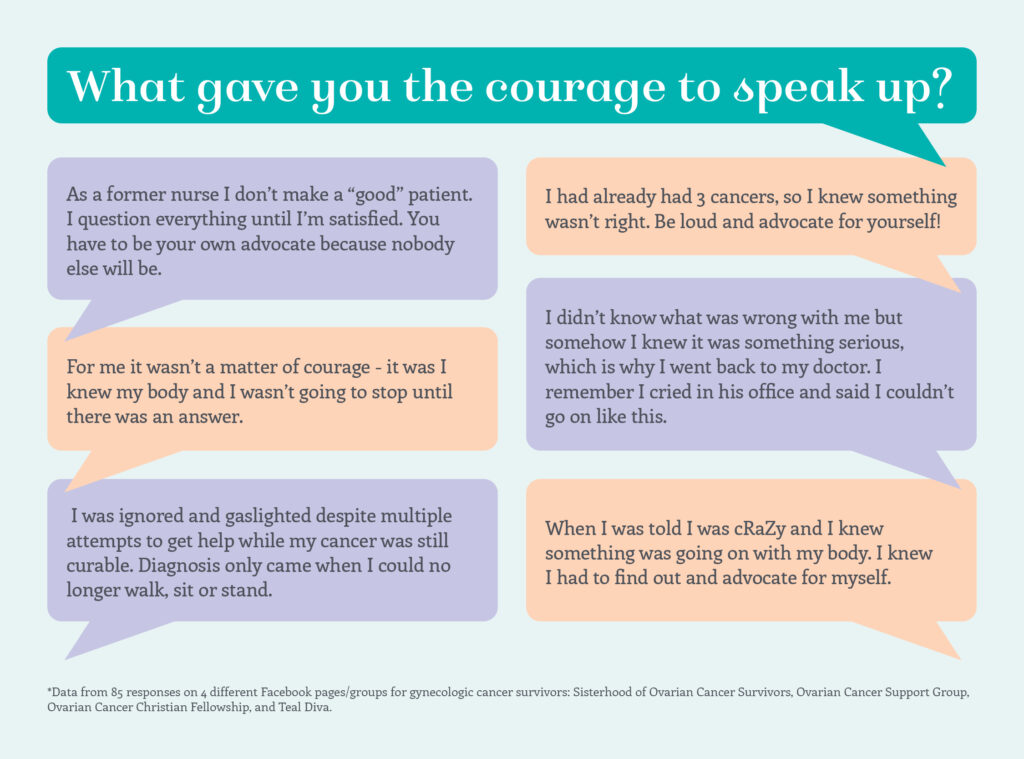
She trusted that instinct and kept pushing for answers.
Her diagnosis initially came back as stage 1 vulvar cancer. Surgery followed, but pathology revealed cancer in her lymph nodes, advancing her diagnosis to stage 3. Despite aggressive treatment, the cancer would later recur and spread, ultimately progressing to stage 4.
“There is life after cancer.”
From that point forward, Pippa’s life became shaped by treatment decisions, recovery, and resilience. She underwent radiation, chemotherapy, and multiple surgeries—including a total pelvic exenteration. Hospital stays were long. Recovery was exhausting. Everyday routines had to be relearned.
Throughout it all, support became essential. Pippa credits her husband as her constant anchor, alongside family, friends, coworkers, and an employer who showed remarkable patience and compassion. Their presence made the hardest moments survivable.


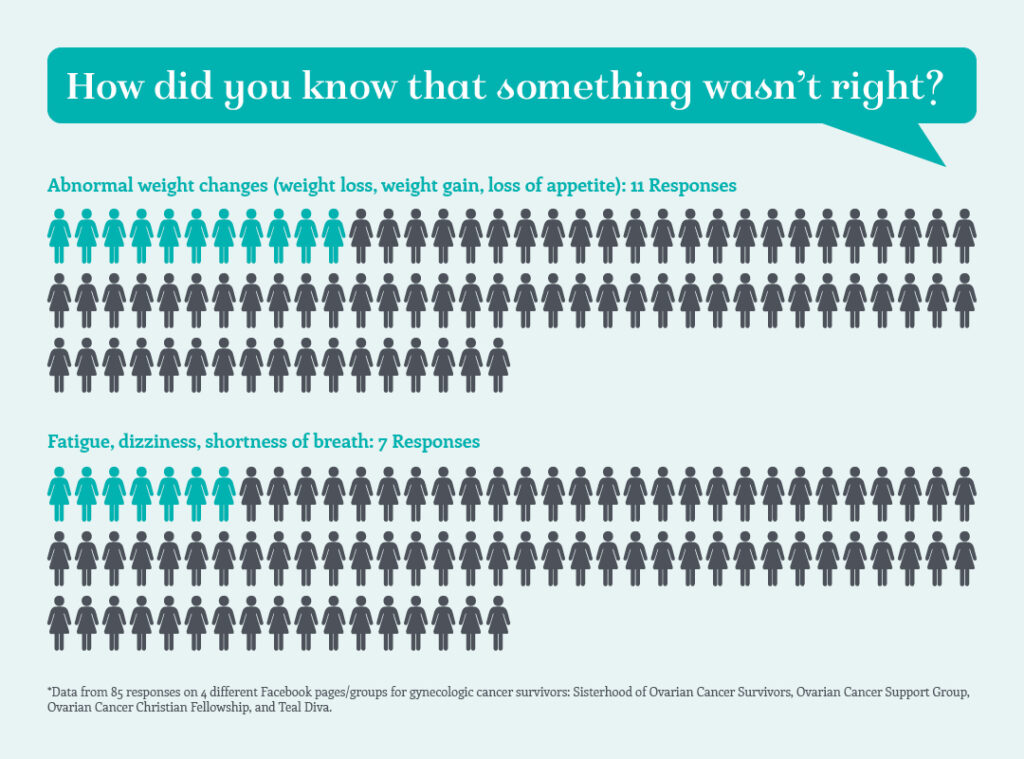
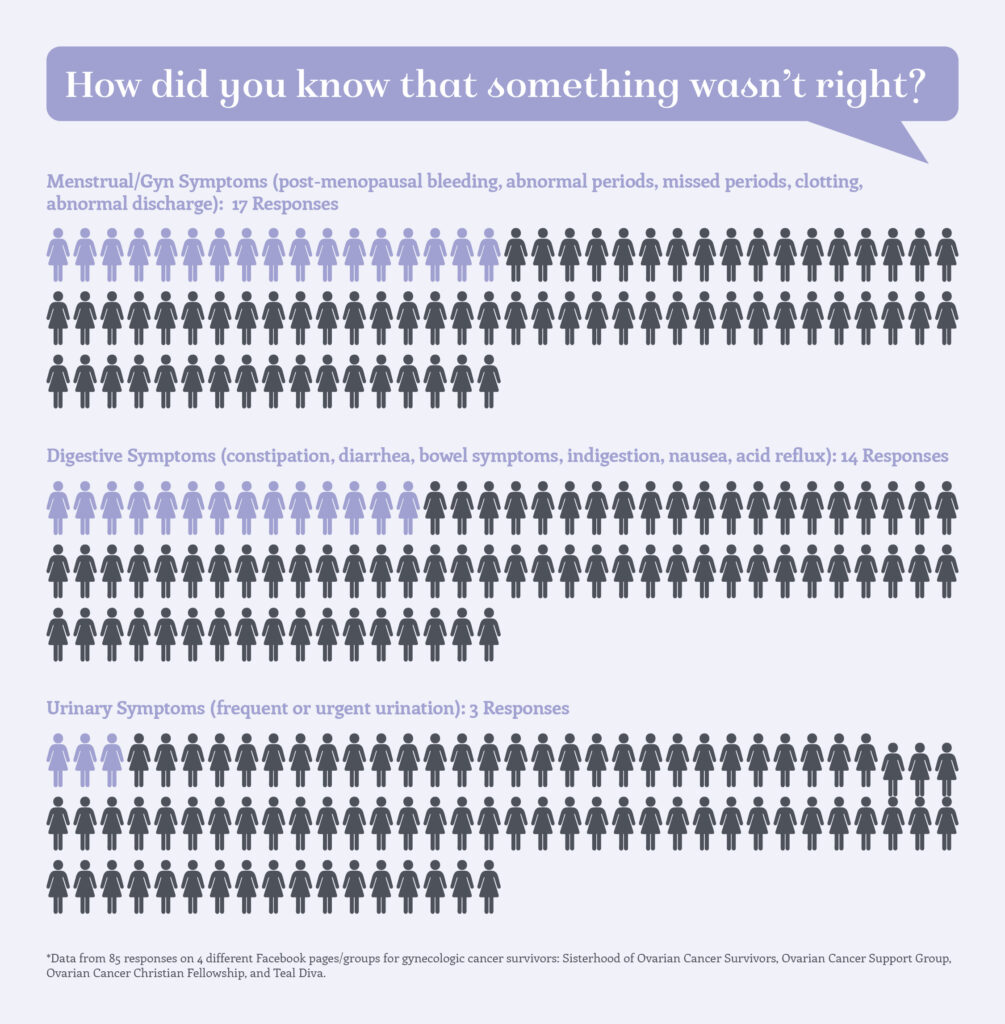
The First Warning Signs
The earliest red flag was a sore, itchy patch inside her left labia that steadily worsened. Creams and medications offered no relief. Over time, it became painful to walk, sit, or stand. Bleeding and discomfort during sex followed, until intimacy became unbearable.
That was when she made the appointment.
Her doctor recognized the symptoms immediately and ordered a biopsy. Even before results came back, Pippa knew the truth. The biopsy confirmed vulvar cancer—painful, validating, and life-altering all at once.
Her diagnosis was upgraded to stage 3. Pippa wasn’t surprised. Her instincts had already prepared her.
Treatment followed quickly: weeks of radiotherapy and chemotherapy that drained her physically and emotionally. Recovery was lonely at times, marked by fatigue and the need for quiet, but she pushed through one day at a time.
Recurrence and a Defining Choice
In early 2024, symptoms returned. More biopsies. More surgeries. Then scans revealed internal recurrence—in her groin and later her lung. Radiation was no longer an option. Surgery was considered too risky. The remaining recommendation was high-dose chemotherapy.
Pippa declined.
“When treatment options dwindled, I chose quality of life over harsher intervention.”
Later that year, Pippa underwent a total pelvic exenteration—one of the most extensive surgeries performed. Organs were removed. Two stomas became part of her daily life. Recovery required weeks in the hospital and learning to walk again.
The physical toll was immense, but she adapted. Life slowed. Energy became precious. Perfection gave way to presence.
Fatigue, chronic pain, osteoarthritis, and lymphedema remain. Yet Pippa has found peace in adjusting expectations and focusing on what truly matters.
Support, Acceptance, and Living Fully
Emotionally, the journey has been just as complex. Counseling helped Pippa navigate being told her cancer was terminal. Her greatest fear was not death—but leaving her husband behind.
Over time, she learned to live with uncertainty.

Today, Pippa finds meaning in small joys: walking her dog, time in nature, quiet moments with her husband. She channels her experience into advocacy, speaking openly about vulvar cancer and helping other women recognize early symptoms.
She reminds others that embarrassment should never delay care—and that advocacy saves lives.
“A few minutes of embarrassment are worth the rest of your life.”
Pippa’s story challenges traditional ideas about survival. It is not about cure or timelines—it is about autonomy, dignity, and choosing how to live. Her experience reminds us that listening to our bodies, trusting our instincts, and advocating for care can change everything.
Citation
Sanchez, C. (Ed.). (2025, November 2). Choosing life on her terms: Pippa’s Stage 4 vulvar cancer story. The Patient Story. Retrieved from https://thepatientstory.com/patient-stories/vulvar-cancer/metastatic-vulvar-cancer/pippa-s/